Health
Report Urges Major Steps to Help Victims of Cardiac Arrest

LAURAN NEERGAARD, AP Medical Writer
WASHINGTON (AP) — Would you know what to do if you see someone collapse, not breathing — a loved one at home, a co-worker at the office, a stranger on the street? Far too many Americans die of cardiac arrest, and now a major new report urges a national campaign to improve survival in part by making sure more bystanders know how to help.
Every year, about 395,000 people suffer cardiac arrest in their homes or other non-hospital settings — and less than 6 percent of them survive, the Institute of Medicine estimated Tuesday.
That’s not the whole toll: An additional 200,000 cardiac arrests occur in hospitals every year, and even there only a quarter of patients survive, the report found.
Cardiac arrest is not a heart attack — it’s worse. It means the heart abruptly stops beating, its electrical activity knocked out of rhythm. CPR can buy critical time if it’s started immediately, but Tuesday’s report concludes the nation must take key steps to give victims a better shot.
“Cardiac arrest survival rates are unacceptably low,” said Dr. Robert Graham of George Washington University, who chaired the IOM committee’s investigation. “There is a lot an individual can do to assist somebody if they witness one, and to work with their communities to improve the system of response.”
What to do may sound straightforward: Call 911, and then start quick, hard compressions of the person’s chest until trained responders arrive. If a device called an AED — an automated external defibrillator — is available, use it.
In reality, the IOM committee said fear, not understanding what cardiac arrest is, lack of first-aid training and concern about legal liability can hamper response and cost precious time. Each year, less than 3 percent of the U.S. population receives training in CPR or defibrillator use, while some European countries mandate training, the report found.
Moreover, there are wide disparities in outcomes: One study found that survival ranged from about 8 percent to 40 percent across 10 different communities.
On Tuesday, the IOM called for a major public education effort to teach people how to recognize and react to cardiac arrest — including making CPR training a graduation requirement for high school. According to the American Heart Association, Connecticut just became the 24th state to pass legislation to do that.
State and local health departments should team with health groups to create “a culture of action,” the IOM recommended. It also urged employers to stock defibrillators and train workers to use them, and expanded access to CPR training for people over age 65 and their caregivers.
Good Samaritan laws provide varying legal protection by state. At the same time, laymen shouldn’t feel they have to provide perfect care, said IOM committee member Dr. Tom Aufderheide of the Medical College of Wisconsin.
“Any CPR and any early defibrillation delivered by the public is better than no care at all,” he said.
Other recommendations:
—The Centers for Disease Control and Prevention should create a national registry of cardiac arrest. There are no good statistics on this killer, the IOM said, calling its own numbers the best available estimates. A registry would track outcomes so communities could take steps to improve. The CDC said it will review the recommendation.
—National standards are needed for emergency medical systems, to ensure that 911 callers are talked through how to provide CPR.
—The National Institutes of Health should expand research for better treatments. Defibrillators attempt to shock the heart back into rhythm so it can resume beating, but most out-of-hospital cardiac arrests aren’t the kind of abnormal rhythms that a shock can fix, said IOM committee member Dr. Lance Becker of the University of Pennsylvania. Yet the report found the NIH spends far less on cardiac arrest research than on other cardiovascular problems.
—Hospitals should have to meet national accreditation standards on cardiac arrest care. Survival of patients who suffer cardiac arrest while hospitalized for some other reason can vary by 10 percent between hospitals, IOM found.
Improvement is possible, the IOM found, calling some communities examples. In King County, Washington, there’s a 62 percent survival rate among patients with a specific shockable form of cardiac arrest if they collapse in front of someone. Policymakers there have spent decades studying what care works best, and getting bystanders and professionals on board with response practices.
The American Heart Association — which along with the American Red Cross, American College of Cardiology and the federal government had requested the IOM’s study — welcomed the recommendations.
Cardiac arrest is “the most critically ill state a human being can be in,” said Dr. Robert W. Neumar of the University of Michigan, who chairs a heart association emergency care committee. The nation needs to create a culture where “if someone collapses in front of you with cardiac arrest, it’s your obligation to help.”
Copyright 2015 The Associated Press. All rights reserved. This material may not be published, broadcast, rewritten or redistributed.
Bay Area
Mind, Body, and Spiritual Well-Being for Women Addressed in NAACP Forum in Oakland
The Women In The NAACP Oakland Branch is proud to announce the upcoming “Total You – Mind, Body, and Spirit Women’s Health Forum” scheduled for April 27 at Acts Full Gospel Church. Running from 9 a.m.-2 p.m. at 1034 66th Ave., this forum aims to provide an empowering platform for women to engage in discussions, gain knowledge, and access resources pertaining to their health and well-being.

Special to The Post
The Women In The NAACP Oakland Branch is proud to announce the upcoming “Total You – Mind, Body, and Spirit Women’s Health Forum” scheduled for April 27 at Acts Full Gospel Church.
Running from 9 a.m.-2 p.m. at 1034 66th Ave., this forum aims to provide an empowering platform for women to engage in discussions, gain knowledge, and access resources pertaining to their health and well-being.
The forum will feature renowned experts, healthcare professionals, and advocates from Genentech, John Muir Health, Sutter Health of The East Bay, Kaiser Permanente, and the Alameda County Public Health Department.
Our expert panel will address various aspects of women’s health, including physical, mental, and emotional well-being, and healthy relationships. The forum will encompass a wide range of topics such as breast cancer, menopause, reproductive health, nutrition, mental health awareness, preventive care, and much more.
Participants will have the opportunity to attend informative sessions, interactive workshops, and panel discussions led by experts in their respective fields. Additionally, there will be wellness activities, screenings, and informational booths offering valuable resources and support.
This forum is open to women of all ages and backgrounds, encouraging inclusivity and diversity in the conversation surrounding women’s health. Whether you’re seeking information for yourself, a loved one, or simply looking to connect with other women, this event promises to be enlightening and empowering.
For more information and to register for the Total You Women’s Health Forum, please visit https://www.naacpoakland.org/ or contact Dr. Delores Thompson. WIN chairwoman at (510) 328-3638.
The Women In The NAACP Oakland Branch is dedicated to empowering women, and young teen girls. We look forward to your participation in this important event.
To register, go to https://www.naacpoakland.org/events/the-total-you-womens-health-forum
Alameda County
Oakland Conducts Its Biennial ‘Point in Time’ Homelessness Count
Oakland, along with other cities in Alameda County, conducted their biennial ‘Point In Time’ census count on Feb. 1 to gain a thorough understanding of the size and dispersion of the homeless population in the region. The Point In Time (PIT) count is federally required by the Housing and Urban Development Department as a requirement to receive funding and resources to tackle homelessness in the area.

By Magaly Muñoz
Oakland, along with other cities in Alameda County, conducted their biennial ‘Point In Time’ census count on Feb. 1 to gain a thorough understanding of the size and dispersion of the homeless population in the region.
The Point In Time (PIT) count is federally required by the Housing and Urban Development Department as a requirement to receive funding and resources to tackle homelessness in the area.
David Modersbach, Grants Manager of Alameda County Health Care for the Homeless program, said that the methodology this time around was different, as this count had a much more personal “lived experience” aspect that previous counts did not have.
In 2022, the county relied more on statistical extrapolation and assumptions, but this year’s survey questionnaires allowed for details on substance abuse issues, how long someone has been living without proper housing, what resources people are in need of and much more.
“[The PIT count is] a critical opportunity for the county, Continuum of Care, and cities to understand the magnitude of homelessness in Alameda County. [The count] enables us to better allocate resources and implement effective programs to tackle this issue head-on in a compassionate and inclusive way,” Modersbach said.
St. Mary’s Center was one of the many meeting hubs across the county that hosted volunteers and community officials the morning of the count. The organization has been deeply involved in the effort to provide resources for unhoused people and others in need.
St. Mary’s is a nonprofit in West Oakland that helps seniors and preschool families with food and housing. Last year, the organization helped about 50 seniors find housing after they had fallen on hard times.
Sharon Cornu, executive director of St. Mary’s, said a lot of the older couples and individuals that come into the center have borne the brunt of the skyrocketing cost of living in the Bay Area. The most recent influx of seniors St. Mary’s has seen coming in for help has been made up of people who were evicted when the COVID-19-related moratorium on rent payment ended.
“Seniors are the fastest growing segment of the unhoused and the incredibly high cost of housing is driving them to the streets,” Cornu said.
Among the volunteers were workers with Operation Dignity, a nonprofit organization that helps veterans and those living on the street find shelter, transitional housing and supportive services.
“These are our stomping grounds,” Ivan Magana, program manager for Operation Dignity said.
Magana stated that his team was extremely familiar with the people residing in the encampments they were conducting the count in since Operation Dignity made many visits to these areas while doing community outreach. He said they had even informed some of the unhoused people they knew about the count a few days prior so they would not be alarmed when the enumerators showed up early in the morning to conduct the count.
Not everyone got the memo though, as the volunteers encountered an almost violent situation around the 6 a.m. when a young woman living in a bus yelled at the Operation Dignity workers to leave her alone.
Luckily, the three-year experience Mangana has working with Operation Dignity and his knowledge of therapeutic health services, equipped him with the techniques needed to deescalate the tension. The woman soon realized who the volunteers were and apologized, he said.
Another volunteer and Operation Dignity worker, Yolanda Kirkpatrick, noted that she was initially hesitant because of the early schedule. She felt the time deterred others from participating, too.
Her prediction would come true as the hours went on and they continued to walk along 24th St in downtown Oakland and there was very little activity on the streets.
The volunteers shared similar sentiments. Although the community the people they were engaging for the count and surveys encounter tend to distrust outsiders, the PIT count was necessary for the city to receive the appropriate level of federal funds to address a crisis that is spiraling out of control in California.
A full analysis and report of the count will be made available in the summer.
Community
For Cervical Cancer Month, Medical Community Focused on Education
January was Cervical Cancer Awareness Month. Physicians, advocates and others in the medical community commemorated the month by raising awareness about a form of cancer they say is highly preventable and treatable. Cervical cancer is caused by a virus called the human papillomavirus (HPV) and it develops slowly over time but can be prevented with proper care in girls as young as 13 years old.

By Magaly Muñoz
January was Cervical Cancer Awareness Month.
Physicians, advocates and others in the medical community commemorated the month by raising awareness about a form of cancer they say is highly preventable and treatable.
Cervical cancer is caused by a virus called the human papillomavirus (HPV) and it develops slowly over time but can be prevented with proper care in girls as young as 13 years old.
Sonia Ordonez, an OBGYN and gynecology surgeon at Kaiser Permanente, stated that as soon as people with cervixes reach the maturity reproductive age, they should start taking preventative measures like getting the HPV vaccine. The vaccine involves a series of two-doses for people aged 9 through 14 or three-doses for people 15 through 45 years old.
“I see a lot of young women who can’t remember or may not have gotten [the vaccine] when they were younger, or maybe got one, but we can give them the series of vaccines and restart at any point in time,” Ordonez said.
She said that cervical cancer is not the only cancer caused by HPV. Strains of the virus can also lead to throat, anal and penile cancers.
Screening is also an effective way to check for cervical cancer and should be done every three years after someone turns 21, doctors recommend. It is best to start as early as possible to catch occurrences early.
Ordonez said that this cancer is also more likely found in people of color and has led to more deaths overall.
A Mayo Clinic article published last month stated that Black women are more likely to be diagnosed and die of cervical cancer, compared to White women in the U.S.
2,000 Black women are diagnosed every year with cervical cancer and 40% die as a result.
“This disparity is not due to genetic differences among White, Black or Hispanic women, but rather related to systemic racism, access to healthcare and socioeconomic factors,” Dr. Olivia Cardenas-Trowers, a Mayo Clinic urogynecologist, said in the article.
Ordonez stated that immigrant women are also highly susceptible to the cancer, as many Latin American countries may not have accessibility to screenings or lack of insurance makes it harder for them to get tested.
Hispanic women are 40% more likely to be diagnosed with cervical cancer, and 30% more likely to die from it, as compared to non-Hispanic White women, according to the Office of Minority Health.
Family medicine physician, Joy Anyanwu, stated that the pandemic contributed to hesitancy about getting cervical cancer screenings among some women. Other factors are people’s aversion to vaccines, parents not wanting to believe that their children are or will become sexually active, and doubt about the overall effectiveness of the vaccine.
“The vaccine is very safe — over 97% effective in preventing cervical cancer,” Anyanwu said. “Even if you aren’t having sex, the earlier you start would actually help.”
Anyanwu said she understands that parents might not want to ask questions about their children’s reproductive health, but it’s a mindset that can be a barrier to having important conversation about prevention or care.
To keep families their families and communties healthy, the doctor emphasized that people should prioritize keeping up with their vaccine series and going to screenings every year.
-

 Activism4 weeks ago
Activism4 weeks agoOakland Post: Week of March 27 – April 2, 2024
-

 #NNPA BlackPress4 weeks ago
#NNPA BlackPress4 weeks agoFrom Raids to Revelations: The Dark Turn in Sean ‘Diddy’ Combs’ Saga
-

 #NNPA BlackPress4 weeks ago
#NNPA BlackPress4 weeks agoCOMMENTARY: D.C. Crime Bill Fails to Address Root Causes of Violence and Incarceration
-

 #NNPA BlackPress4 weeks ago
#NNPA BlackPress4 weeks agoCOMMENTARY: Lady Day and The Lights!
-

 #NNPA BlackPress4 weeks ago
#NNPA BlackPress4 weeks agoMayor, City Council President React to May 31 Closing of Birmingham-Southern College
-

 #NNPA BlackPress4 weeks ago
#NNPA BlackPress4 weeks agoBaltimore Key Bridge Catastrophe: A City’s Heartbreak and a Nation’s Alarm
-

 #NNPA BlackPress4 weeks ago
#NNPA BlackPress4 weeks agoBaltimore’s Key Bridge Struck by Ship, Collapses into Water
-
 #NNPA BlackPress4 weeks ago
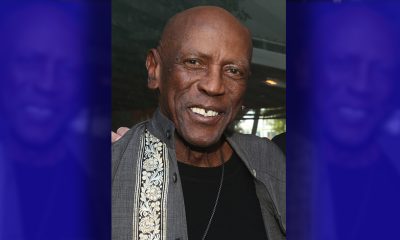
#NNPA BlackPress4 weeks agoBeloved Actor and Activist Louis Cameron Gossett Jr. Dies at 87