Health
Redefining Chronic Fatigue with Better Diagnosis, New Name

Dr. Ellen Wright Clayton, left, chair of the Committee on Diagnostic Criteria for Myalgic Encephalomyelitis/Chronic Fatigue Syndrome speaks during an open meeting at the Institute of Medicine in Washington, Tuesday, Feb. 10, 2015. (AP Photo/Susan Walsh)
LAURAN NEERGAARD, AP Medical Writer
WASHINGTON (AP) — Doctors are getting a new way to diagnose chronic fatigue syndrome — and influential government advisers say it’s time to replace that hated name, too, to show it’s a real and debilitating disease.
The Institute of Medicine on Tuesday called on doctors to do a better job diagnosing an illness that may affect up to 2.5 million Americans, and it set five main symptoms as the criteria.
And the IOM’s choice of a new name — Systemic Exertion Intolerance Disease, or SEID — reflects a core symptom, that exertion can wipe patients out.
“This is not a figment of their imagination,” said Dr. Ellen Wright Clayton of Vanderbilt University’s Center for Biomedical Ethics and Society, who chaired the IOM panel. “These patients have real symptoms. They deserve real care.”
Here are some things to know about the disorder:
WHATEVER IT’S CALLED, WHAT IS THIS ILLNESS?
Its hallmark is persistent and profound fatigue where, on a bad day, a simple activity like grocery shopping can put someone to bed. It’s often accompanied by memory problems or other symptoms.
Laura Hillenbrand, author of best-sellers “Unbroken: A World War II Story of Survival, Resilience, and Redemption” and “Seabiscuit: An American Legend,” has put a public face to the confusing illness.
“Well, in the years in which I’ve been exhausted it’s been something where I’ve had to drag myself to my computer or to my telephone to do interviews,” she said on CBS’ “Face the Nation” last December.
While working on her book “Unbroken,” she said that over a two-year stretch, she was “unable to leave the house a single time, because I simply wasn’t strong enough to walk to the car to get out of the house.”
GETTING DIAGNOSED HAS LONG BEEN A PROBLEM
Between 836,000 and 2.5 million Americans suffer from the disorder, and most have no formal diagnosis, Tuesday’s report estimated.
Patients flooded the IOM with stories of years of misdiagnosis or even being dismissed by skeptical doctors as having a psychological problem instead. There’s no medical test for the disorder, leaving doctors to rule out other possible causes for the exhaustion. No one knows what causes it.
There’s no specific treatment, and the IOM found less than a third of medical schools teach about the disease.
WHAT’S NEW
The federal government asked the independent Institute of Medicine to investigate the state of chronic fatigue diagnosis. Tuesday, the panel issued new criteria that it said should enable any physician to tell which patients are affected.
Diagnosis requires three core symptoms: Fatigue and reduction in pre-illness levels of activity that last for more than six months, the post-exertion worsening, and sleep that is unrefreshing despite exhaustion.
Also, patients must have at least one other symptom: Cognitive impairment, sometimes described as “brain fog,” or what’s called orthostatic intolerance — meaning symptoms improve when lying down and patients find it hard to stay upright for long.
WHAT’S IN A NAME?
Patients have long sought a change to a name they say belittles their suffering. Some groups already had begun using a more tongue-twisting name — myalgic encephalomyelitis/chronic fatigue syndrome, or ME/CFS. Tuesday’s report rejected that option, saying not all patients have the muscle pain and brain or spinal cord inflammation that medical jargon reflects.
It’s too early to know if the alternative name proposed Tuesday will catch on. But just including the word “disease” instead of “syndrome” is important, said Carol Head, who leads the Solve ME/CFS Initiative, the largest advocacy organization.
“Having called this serious disease by an inappropriate and frankly insulting name is one of the factors that kept doctors, friends, family members, even employers from affording it the seriousness it deserves,” she said.
WHAT TO DO AFTER DIAGNOSIS
Doctors may not know how to cure the disorder, but there are treatments for individual symptoms, noted committee member Dr. Lucinda Bateman of the Fatigue Consultation Clinic in Salt Lake City.
Moreover, the IOM said there’s been “a paucity of research” into the causes, treatments, even the natural history of the disease to figure out who may get better over time. At Solve ME/CFS, Head said the report should spur more research funding.
WHAT HAPPENS NEXT?
The IOM advised the government to develop a toolkit to help doctors diagnose the disease, and to make sure the disorder is assigned a specific medical billing code. The government is reviewing the recommendations.
Committee members are spreading the word about the diagnostic criteria in medical journals, and the institute’s web site, www.iom.edu, eventually will post a physician guide.
Copyright 2015 The Associated Press. All rights reserved. This material may not be published, broadcast, rewritten or redistributed.
Community
Report: Black Women Doctors are Underrepresented in Health Care Sector
Physician retention in California has decreased over the years for women doctors of color, a report by the Physicians for a Healthy California stated. According to the report, women physicians are more likely to experience burnout than their male counterparts, a trend that worsened during the COVID-19 pandemic.

By California Black Media
Physician retention in California has decreased over the years for women doctors of color, a report by the Physicians for a Healthy California stated.
According to the report, women physicians are more likely to experience burnout than their male counterparts, a trend that worsened during the COVID-19 pandemic.
The report states that Black and Latino physicians are underrepresented in the healthcare industry. Only 2.8% of physicians are Black and 5.5% are Latino across the state of California.
It also noted that women doctors of color are often assigned to serve in vulnerable and under-resourced communities.
“It is critical for health care organizations to implement effective strategies focused on the retention of this important group of clinicians,” the report stated.
Women doctors of color face career dissatisfaction, contributing to the low retention rates in California’s healthcare industry. The burnout particularly experienced by female doctors of color stems from workplace harassment and perceived lack of value at work.
Additionally, moral injury was another key factor driving women physicians of color away from the workforce. Unlike burnout, moral injury is defined as “the betrayal of what’s right by someone who holds legitimate authority in a high-stakes situation.”
Currently, two of the nine California regions used in the framework of the report — the Inland Empire and San Joaquin Valley — have less than 50 primary care doctors. Physician shortages are projected to get worse over the next few years.
By 2030, the report indicates, the demand for physicians will exceed the supply by at least 12%.
Community
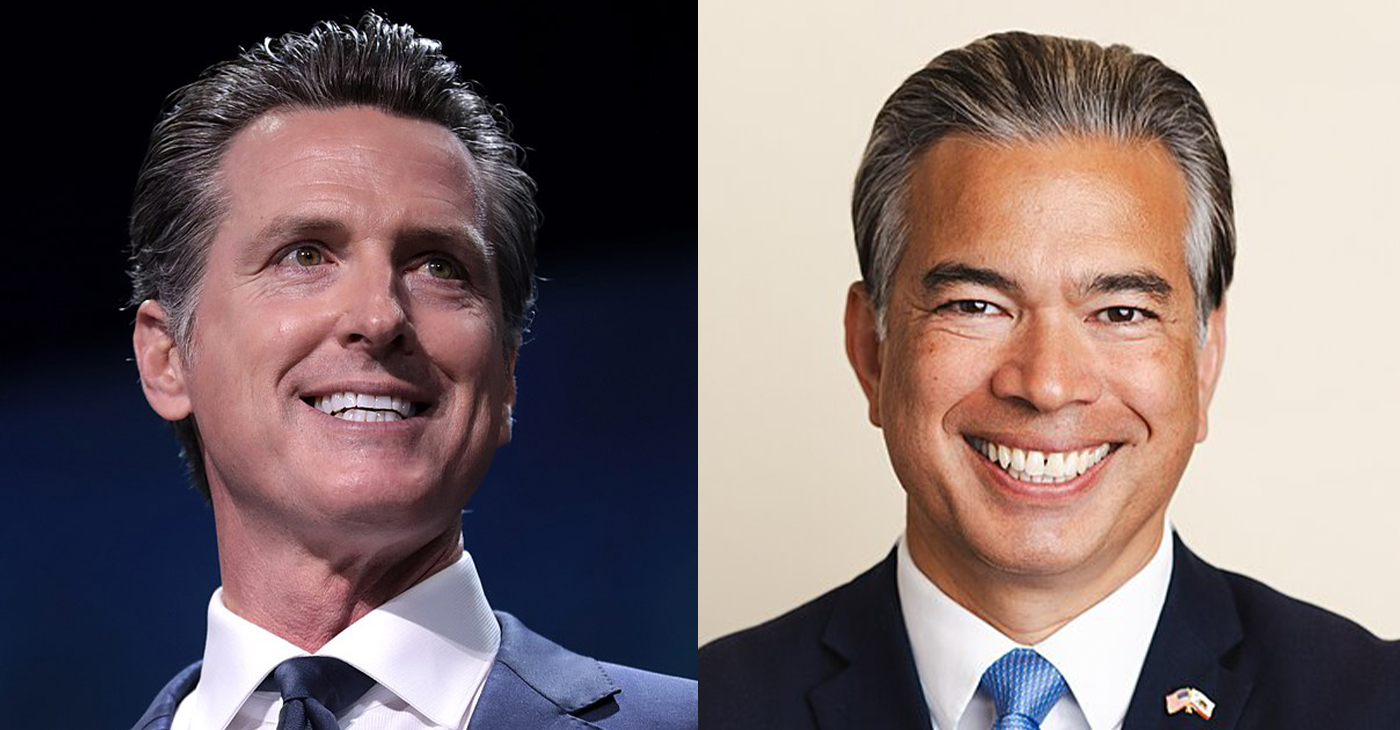
Gov. Newsom, Attorney General Bonta Back Bill to Allow California to Host Arizona Abortion Care
Gov. Gavin Newsom and Attorney General Rob Bonta announced last week that they are backing a bill introduced by the state legislative women’s caucus that would allow Arizona-based doctors to provide abortion care in California to patients from Arizona. Senate Bill (SB) 233 was authored in response to the Arizona Supreme Court’s decision on April 9 that an 1864 ban on abortion in the state is enforceable.
By California Black Media
Gov. Gavin Newsom and Attorney General Rob Bonta announced last week that they are backing a bill introduced by the state legislative women’s caucus that would allow Arizona-based doctors to provide abortion care in California to patients from Arizona.
Senate Bill (SB) 233 was authored in response to the Arizona Supreme Court’s decision on April 9 that an 1864 ban on abortion in the state is enforceable. The bill also aims to counter growing support for anti-abortion legislation in states with Republican-majority legislatures since Roe v. Wade was overturned, according to supporters.
“California will not sit idly by. We’re urgently moving legislation to allow Arizona doctors to provide safe and reliable reproductive care to Arizonans here in California,” Newsom said.
Sen. Nancy Skinner (D-Berkeley), chair of the California Legislative Women’s Caucus said that abortion bans are based on laws that set women back to a time when they had limited human rights.
“Anti-abortion forces have resurrected a dead law passed at a time when women couldn’t vote and husbands beating their wives was lawful,” Skinner said.
On April 24, the Arizona House of Representatives voted to repeal the 1864 abortion ban. It now moves to the Arizona Senate for deliberation.
Bay Area
Mind, Body, and Spiritual Well-Being for Women Addressed in NAACP Forum in Oakland
The Women In The NAACP Oakland Branch is proud to announce the upcoming “Total You – Mind, Body, and Spirit Women’s Health Forum” scheduled for April 27 at Acts Full Gospel Church. Running from 9 a.m.-2 p.m. at 1034 66th Ave., this forum aims to provide an empowering platform for women to engage in discussions, gain knowledge, and access resources pertaining to their health and well-being.

Special to The Post
The Women In The NAACP Oakland Branch is proud to announce the upcoming “Total You – Mind, Body, and Spirit Women’s Health Forum” scheduled for April 27 at Acts Full Gospel Church.
Running from 9 a.m.-2 p.m. at 1034 66th Ave., this forum aims to provide an empowering platform for women to engage in discussions, gain knowledge, and access resources pertaining to their health and well-being.
The forum will feature renowned experts, healthcare professionals, and advocates from Genentech, John Muir Health, Sutter Health of The East Bay, Kaiser Permanente, and the Alameda County Public Health Department.
Our expert panel will address various aspects of women’s health, including physical, mental, and emotional well-being, and healthy relationships. The forum will encompass a wide range of topics such as breast cancer, menopause, reproductive health, nutrition, mental health awareness, preventive care, and much more.
Participants will have the opportunity to attend informative sessions, interactive workshops, and panel discussions led by experts in their respective fields. Additionally, there will be wellness activities, screenings, and informational booths offering valuable resources and support.
This forum is open to women of all ages and backgrounds, encouraging inclusivity and diversity in the conversation surrounding women’s health. Whether you’re seeking information for yourself, a loved one, or simply looking to connect with other women, this event promises to be enlightening and empowering.
For more information and to register for the Total You Women’s Health Forum, please visit https://www.naacpoakland.org/ or contact Dr. Delores Thompson. WIN chairwoman at (510) 328-3638.
The Women In The NAACP Oakland Branch is dedicated to empowering women, and young teen girls. We look forward to your participation in this important event.
To register, go to https://www.naacpoakland.org/events/the-total-you-womens-health-forum
-
 Community2 weeks ago
Community2 weeks agoFinancial Assistance Bill for Descendants of Enslaved Persons to Help Them Purchase, Own, or Maintain a Home
-

 Activism4 weeks ago
Activism4 weeks agoOakland Post: Week of April 3 – 6, 2024
-

 Business3 weeks ago
Business3 weeks agoV.P. Kamala Harris: Americans With Criminal Records Will Soon Be Eligible for SBA Loans
-

 Activism3 weeks ago
Activism3 weeks agoOakland Post: Week of April 10 – 16, 2024
-
 Community3 weeks ago
Community3 weeks agoAG Bonta Says Oakland School Leaders Should Comply with State Laws to Avoid ‘Disparate Harm’ When Closing or Merging Schools
-

 Community2 weeks ago
Community2 weeks agoOakland WNBA Player to be Inducted Into Hall of Fame
-

 Community2 weeks ago
Community2 weeks agoRichmond Nonprofit Helps Ex-Felons Get Back on Their Feet
-
 Community2 weeks ago
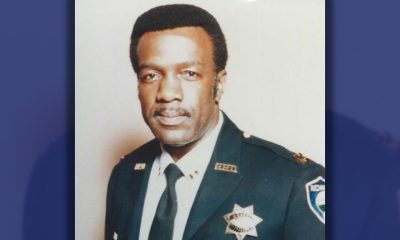
Community2 weeks agoRPAL to Rename Technology Center for Retired Police Captain Arthur Lee Johnson