Community
Addressing Clinician Burnout Through Communal Healing
The COVID-19 pandemic put an extra strain on Black, Indigenous and other people of color (BIPOC) healthcare workers. Over half of all clinicians grapple with burnout symptoms, i.e. fatigue, detachment, depression, mental health decline, and medical errors. The American Medical Association noted that Black physicians (37%) and physicians who identify as two or more races (45%) report the highest rates of burnout onset or increase due to COVID-19.

By Dr. Uzo Nwankpa, DNP, MSN, RN
The COVID-19 pandemic put an extra strain on Black, Indigenous and other people of color (BIPOC) healthcare workers.
Over half of all clinicians grapple with burnout symptoms, i.e. fatigue, detachment, depression, mental health decline, and medical errors.
The American Medical Association noted that Black physicians (37%) and physicians who identify as two or more races (45%) report the highest rates of burnout onset or increase due to COVID-19.
How do we prioritize the well-being of healthcare workers who put their lives on the line for our communities?
As a community health nurse and nursing instructor, I have witnessed burnout symptoms steal the light away from current and future healthcare workers.
I started my nursing journey in an ICU in 2008, facing constant life-or-death scenarios. Surrounded by fatigued, overworked, and undervalued colleagues, I experienced the brokenness of the culture of our medical system. Our healthcare workers need attention.
My journey began 25 years ago, as a young, newly arrived and under-resourced Black immigrant. I faced immense challenges that put me at risk. The relentless dance with assimilation, altering everything from my speech to my mannerisms, was exhausting and lead to years of depression and anxiety.
Family, friends, and my connection to my cultural practices were critical to my healing, empowering me to overcome many obstacles and enabling me to earn my first college degree. Firsthand, I have learned that the societal risk factors we face can be mitigated by protective factors.
One protective factor was reconnecting with my heritage, which provided me with a sense of empowerment. Memories of my ancestral homeland would resurface to remind me of the joys of meaningful interpersonal connection, intentional music to ward off ailments, nourishing meals to rejuvenate the senses, and laughter and tears flowing freely.
Deprivation of these cultural experiences in our modern lives may disrupt our spiritual well-being.
Utilizing African-indigenous cultural wisdom can offer relief among African descendants, Afro-diasporic seeds, and Black folk. In West Africa’s Igbo language, Agwu embodies the inspirer of talent, directing our focus toward artistic pursuits like music, dance, and storytelling.
Tuning into the rhythmic language, the beats of the ogene (metal gong), and the udu (clay pot) charges me up, nurses my cultural longing, and informed the development of the RICHER model-a five-step process to create community healing spaces.
Communal healing sessions utilize this model to support BIPOC healthcare workers in being seen, heard, and affirmed, and incorporates indigenous African healing practices like music, dance, mindfulness, storytelling, and expressivity. These communal sessions yield transformative results, as participants emerge feeling connected, lighter, and inspired to re-engage their restorative work.
Such self-care and strong interpersonal relationships are vital, and the onus shouldn’t fall on individuals alone. Organizations that employ healthcare workers must proactively prioritize well-being and burnout prevention initiatives. At the community level, policies and funding that support mental and emotional well-being are necessary to address this national priority.
Amid the pervasive issue of burnout, communal healing stands out as a beacon of hope and source of rejuvenation. By nurturing caregivers, revitalizing minds, and reigniting spirits, we have the opportunity to reshape the future for our clinicians and communities. Together, let’s revitalize our healthcare environment and elevate healthcare workers to optimal well-being in mind, body, and spirit.
Author Bio
Dr. Uzo Nwankpa is the founder and CEO of Wellness Promoters LLC (ww.wellnesspromoters.net), which partners with organizations to address clinician burnout. Dr. Uzo’s expertise lies in community healing sessions, especially for historically-marginalized community and healthcare workers.
Dr. Uzo is a collaborator of the Bay Area Chapter Association of Black Psychologists (BACABPsi), a healing resource committed to providing the Post Newspaper readership with monthly discussions about critical issues in Black Mental Health. Readers are welcome to contact us at bayareaabpsi@gmail.com and join us at our monthly chapter meetings every third Saturday via Zoom.
Activism
Oakland Post: Week of April 24 – 30, 2024
The printed Weekly Edition of the Oakland Post: Week of April 24 – 30, 2024

To enlarge your view of this issue, use the slider, magnifying glass icon or full page icon in the lower right corner of the browser window. ![]()
Alameda County
DA Pamela Price Stands by Mom Who Lost Son to Gun Violence in Oakland
Last week, The Post published a photo showing Alameda County District Attorney Pamela Price with Carol Jones, whose son, Patrick DeMarco Scott, was gunned down by an unknown assailant in 2018.
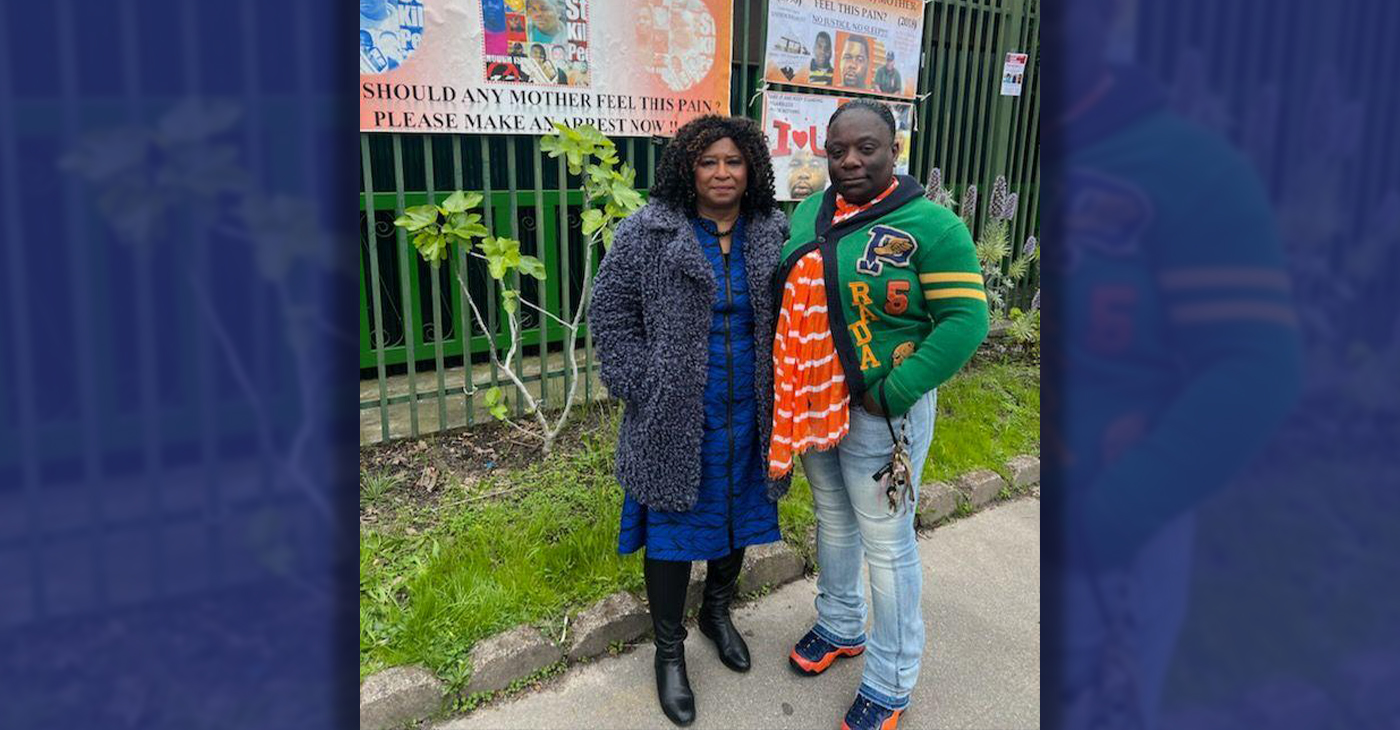
Publisher’s note: Last week, The Post published a photo showing Alameda County District Attorney Pamela Price with Carol Jones, whose son, Patrick DeMarco Scott, was gunned down by an unknown assailant in 2018. The photo was too small for readers to see where the women were and what they were doing. Here we show Price and Jones as they complete a walk in memory of Scott. For more information and to contribute, please contact Carol Jones at 510-978-5517 at morefoundation.help@gmail.com. Courtesy photo.
City Government
Vallejo Welcomes Interim City Manager Beverli Marshall
At Tuesday night’s Council meeting, the Vallejo City Council appointed Beverli Marshall as the interim city manager. Her tenure in the City Manager’s Office began today, Wednesday, April 10. Mayor Robert McConnell praised Marshall’s extensive background, noting her “wide breadth of experience in many areas that will assist the City and its citizens in understanding the complexity of the many issues that must be solved” in Vallejo.

Special to The Post
At Tuesday night’s Council meeting, the Vallejo City Council appointed Beverli Marshall as the interim city manager. Her tenure in the City Manager’s Office began today, Wednesday, April 10.
Mayor Robert McConnell praised Marshall’s extensive background, noting her “wide breadth of experience in many areas that will assist the City and its citizens in understanding the complexity of the many issues that must be solved” in Vallejo.
Current City Manager Michael Malone, whose official departure is slated for April 18, expressed his well wishes. “I wish the City of Vallejo and Interim City Manager Marshall all the best in moving forward on the progress we’ve made to improve service to residents.” Malone expressed his hope that the staff and Council will work closely with ICM Marshall to “ensure success and prosperity for the City.”
According to the Vallejo Sun, Malone stepped into the role of interim city manager in 2021 and became permanent in 2022. Previously, Malone served as the city’s water director and decided to retire from city service e at the end of his contract which is April 18.
“I hope the excellent work of City staff will continue for years to come in Vallejo,” he said. “However, recent developments have led me to this decision to announce my retirement.”
When Malone was appointed, Vallejo was awash in scandals involving the housing division and the police department. A third of the city’s jobs went unfilled during most of his tenure, making for a rocky road for getting things done, the Vallejo Sun reported.
At last night’s council meeting, McConnell explained the selection process, highlighting the council’s confidence in achieving positive outcomes through a collaborative effort, and said this afternoon, “The Council is confident that by working closely together, positive results will be obtained.”
While the search for a permanent city manager is ongoing, an announcement is expected in the coming months.
On behalf of the City Council, Mayor McConnell extended gratitude to the staff, citizen groups, and recruitment firm.
“The Council wishes to thank the staff, the citizens’ group, and the recruitment firm for their diligent work and careful consideration for the selection of what is possibly the most important decision a Council can make on behalf of the betterment of our City,” McConnell said.
The Vallejo Sun contributed to this report.
-

 Activism4 weeks ago
Activism4 weeks agoOakland Post: Week of March 27 – April 2, 2024
-
 #NNPA BlackPress4 weeks ago
#NNPA BlackPress4 weeks agoBeloved Actor and Activist Louis Cameron Gossett Jr. Dies at 87
-
 Community1 week ago
Community1 week agoFinancial Assistance Bill for Descendants of Enslaved Persons to Help Them Purchase, Own, or Maintain a Home
-

 Activism3 weeks ago
Activism3 weeks agoOakland Post: Week of April 3 – 6, 2024
-

 Business2 weeks ago
Business2 weeks agoV.P. Kamala Harris: Americans With Criminal Records Will Soon Be Eligible for SBA Loans
-

 Activism2 weeks ago
Activism2 weeks agoOakland Post: Week of April 10 – 16, 2024
-
 Community2 weeks ago
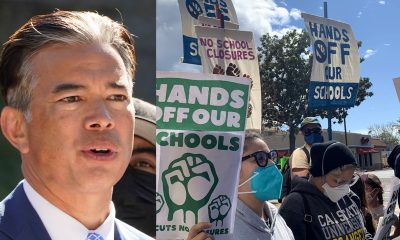
Community2 weeks agoAG Bonta Says Oakland School Leaders Should Comply with State Laws to Avoid ‘Disparate Harm’ When Closing or Merging Schools
-

 Community6 days ago
Community6 days agoOakland WNBA Player to be Inducted Into Hall of Fame